Immunotherapy I: Baby Steps, but No Breakthroughs
Quick Links
Many researchers are eagerly watching for results from Alzheimer’s disease immunotherapy trials. The 7th Clinical Trials on Alzheimer’s Disease (CTAD) conference, held November 20 to 22 in Philadelphia, brought a smattering of updates on these programs, although no big news. Several talks highlighted methodological problems and how researchers are tweaking trial protocols to better measure outcomes and select participants. Biomarker data from the Phase 2 trial of Genentech’s crenezumab reinforced concerns about the standard method of analyzing amyloid PET data, and speakers argued that using a white-matter reference region could help them better detect how the amyloid burden changes over time. Regarding recruitment, other talks stressed the importance of screening for brain amyloid, as it appears that many people who meet cognitive criteria for prodromal AD do not have it. Beyond these technical issues, there were updates on antibody trials, including mostly negative results from a couple of active immunotherapy approaches that have now been scuttled (see Part 5 of this series).
First, consider crenezumab, Genentech’s antibody that binds all forms of Aβ. The Phase 2 results in the mild to moderate ABBY trial were negative overall, with hints of a benefit in patients with milder disease (see Jul 2014 conference news). At CTAD, Stephen Salloway of Butler Hospital, Providence, Rhode Island, presented biomarker data from the Phase 2 BLAZE trial. In this study, 91 participants with mild to moderate AD received either placebo, 15 mg/kg crenezumab injected intravenously, or 300 mg/kg crenezumab subcutaneously for 73 weeks.
On the primary endpoint—PET amyloid imaging—the researchers saw no consistent trend and no difference between the treatment groups on the prespecified analysis. Salloway noted that results from the three scans each patient underwent varied widely, and more than expected. Paul Aisen of the University of California, San Diego, who was not involved with this study, said that Alzheimer’s trials in general still have several biomarker measurement problems that need to be worked out. On the other hand, the secondary endpoint in the BLAZE trial, CSF Aβ, rose slightly but significantly in both treatment groups, in contrast to continued decline in the placebo group, Salloway reported.
On the PET measurement issue, imaging experts have been arguing for some years that the standard method of assessing amyloid PET changes against cerebellar gray matter as a reference region introduces too much noise into the data, especially for longitudinal measurements. White matter, which takes up less tracer, may provide a better contrast (see Feb 2012 conference news). For this reason, Genentech authorized two secondary analyses using white-matter reference regions. Eric Reiman at Banner Alzheimer’s Institute, Phoenix, presented the results from a blinded analysis using a cerebral white-matter reference region that lies at roughly the same plane of the scanner “slice” as the amyloid. In ADNI longitudinal data, this reference region lowers variability and more faithfully reflects the difference between amyloid progressors and non-progressors (see Jul 2014 conference story). With this method, trajectories of amyloid deposition in the crenezumab BLAZE cohorts looked smoother and had less variability, Reiman reported at CTAD. A treatment effect emerged in the IV group, where amyloid appeared to accumulate more slowly, although the effect missed significance. “I believe we are underestimating the treatment effect with crenezumab,” Reiman said.
Gilles Tamagnan at Molecular NeuroImaging, New Haven, Connecticut, led the second exploratory analysis. It used white matter in cerebellum and other subcortical regions as a reference. Salloway discussed this data at CTAD, noting that the findings looked similar to Reiman’s, with the IV treatment group trending toward less amyloid accumulation. As with Reiman’s method, the within-person variability of longitudinal scans dropped.
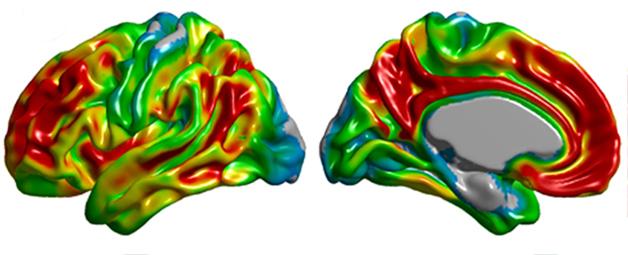
Spatial distribution of amyloid PET tracer binding in Alzheimer's disease. [Image courtesy of Felix Carbonell, Biospective Inc.]
Which method is better? Barry Bedell of McGill University, Montreal, addressed this question in his talk. In an analysis of PET data obtained from ADNI cohorts and participants in Biogen Idec’s Phase 1b trial of the Aβ antibody BIIB0037, white matter in the cerebellum and pons provided the best reference region for discriminating amyloid-negative from amyloid-positive scans, he reported. Bedell told Alzforum that cerebral white matter performed comparably to cerebellar white, but during immunotherapy the former tissue can develop lesions known as ARIA-E, which affect the PET signal. For this reason, a subcortical reference region may be more reliable. However, Bedell stressed that the key was to exclude cerebellar gray matter. “Every time we included cerebellar gray matter, the results were inferior to when we did not. There is a marked increase in accuracy when you exclude it.”
In the crenezumab trial, the hint of a treatment effect occurred only in the IV groups. In the subcutaneous treatment group, which received about half the effective dose as the IV group because not all the injected antibody got into the bloodstream, trajectories resembled those of controls. As a result of these data, the Alzheimer’s Prevention Initiative upped the crenezumab dose administered subcutaneously to the participants in its secondary prevention trial in Colombia to match the IV levels, Reiman said (see May 2012 conference story). Meanwhile, Genentech will continue its high-dose extension trial of crenezumab, and has met with the FDA to discuss whether to develop the antibody further, Salloway said.
Progress reports from other antibody trials focused on patient selection. Philip Scheltens of VU University Medical Center, Amsterdam, detailed baseline data for the ongoing Phase 3 SCarlet RoAD trial of Roche’s monoclonal antibody gantenerumab. Gantenerumab is also being tested in the DIAN-TU prevention trial (see Oct 2012 conference story; Sep 2013 news story). Scheltens’ talk reviewed how screening with the new Dubois criteria (see Part 1 of this series) works out in the reality of a multicenter trial. Roche’s trial enrolls about 800 people with prodromal Alzheimer’s disease. Partway into the screening, it delivers the Free and Cued Selective Reminding Test (FCSRT) to measure if the candidate has a hippocampal memory deficit, and those who meet the cutoff then undergo a lumbar puncture to determine if the deficit is due to underlying Alzheimer’s pathology.
Of 3,000 people screened, 2,290 fell out at some point. Eight hundred and twenty-one scored above the upper cutoff on the FCSRT. Of those who passed this step, 621 more subsequently failed the CSF test, meaning they had an episodic memory deficit but no CSF evidence of AD pathology. Of those 621, roughly two-thirds, or 413, had usable data in the system. Scheltens compared this group of 413 to the baseline trial population. He found that people who failed the CSF screen were younger than the trial population and had a milder cognitive phenotype. They scored better on global cognitive measures such as CDR, ADAS-Cog, and MMSE, as well as on tests of episodic memory and executive function, Scheltens said. Overall, the use of a CSF screen to enrich a prodromal population selected people with greater deficits, he concluded. On the other hand, if the researchers had not screened for amyloid, they would have enrolled those 621 people in the trial, meaning about 43 percent of the participants would have lacked evidence of amyloid pathology.
Similar results were reported on a poster from Jeff Sevigny, Biogen Idec, Cambridge, Massachusetts. For the Phase 1b trial of its therapeutic antibody aducanumab (aka BIIB037), the researchers first screened volunteers using cognitive measures such as the FCSRT, CDR, and MMSE, then measured PET amyloid burden in those who met the cognitive criteria. Out of the first 278 people scanned, about 40 percent had no brain amyloid, similar to Roche’s findings. Likewise, Lilly insiders said at CTAD that screening for the ongoing solanezumab trial in mild AD also fails a significant fraction of cognitively admissible candidates at the subsequent brain amyloid step.
By comparison, in the bapineuzumab and solanezumab trials and ADNI, the number of amyloid-negative participants ran around 15 to 20 percent. Current trials are enrolling an earlier, prodromal population, and thus may pick up more people with cognitive impairment not due to AD, Sevigny suggested in his poster. Supporting this, in Biogen’s screens ApoE4 carriers were more likely to accumulate amyloid, with 80 percent of them testing positive, compared to 43 percent of non-carriers. The findings underscore the importance of amyloid screening for these early trials, Sevigny concluded.
Perhaps the most unexpected passive immunotherapy news came after CTAD closed. Biogen announced on December 2 that it will push aducanumab straight from Phase 1b to Phase 3. The Phase 1 trial enrolled nearly 200 people with prodromal AD and was scheduled to conclude in 2017 (see Apr 2013 conference story). According to an interim analysis, one year of dosing lowered brain amyloid and improved cognition in participants, the company’s Doug Williams claimed at an investor conference. The data will be presented at a research conference next year.—Madolyn Bowman Rogers
References
Therapeutics Citations
News Citations
- Immunotherapy II: Active Approaches Down, New Passive Crops Up
- Crenezumab Disappoints in Phase 2, Researchers Remain Hopeful
- News Focus: 2012 Human Amyloid Imaging Conference
- References and Thresholds—Amyloid Imaging Protocols Debated at AAIC
- NIH Director Announces $100M Prevention Trial of Genentech Antibody
- DIAN Trial Picks Gantenerumab, Solanezumab, Maybe BACE Inhibitor
- NIH Funds Prevention Trials and Translational Studies
- CTAD Shows Alzheimer’s Field Trying to Reinvent Itself
- Safe at 4 Grams? No ARIA at High Dose of Human Aβ Antibody
External Citations
Further Reading
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.